Background: Contemporary treatment of Myeloproliferative Neoplasms (MPNs) has altered their natural history. Frailty, a state of reduced physiologic reserve is prevalent among older individuals, and increases risk for cardiovascular disease (CVD) and other adverse health outcomes. However, little is known about frailty in MPNs. An improved characterization of frailty may inform MPN treatment goals including the impact of treatment on frailty and CVD.
Methods : We utilized the ORCHID database, a multi-centre prospective observational registry of MPN patients. Frailty-related factors collected included: unintentional weight loss (>4kg lost in prior year); grip strength (below 20th percentile for age and sex); Timed Up and Go test (TGUG) greater than 13.5 seconds (indicative of high fall risk); self-reported exhaustion; and cognitive frailty measured by the Digit Symbol Substitution test (DSST). Baseline information on cardiovascular event history was also collected.
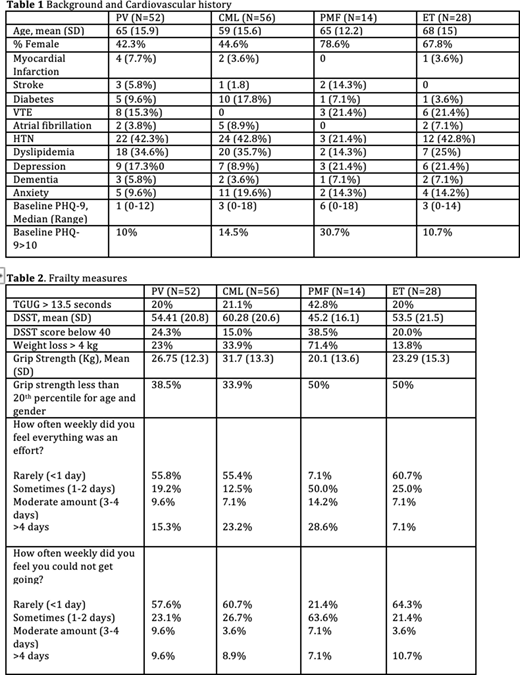
Results: In total, 150 patients were included (56 CML, 28 ET, 14 PMF, 52 PV). Baseline information and past medical history are detailed in Table 1. Cardiovascular events prior to diagnosis were most common in patients with PV (7.7% MI and 5.8% stroke). Past medical history of Venous Thromboembolism (VTE) was more common in Ph-negative MPNs (15.3% PV, 21.4% PMF, 21.4% ET) compared to CML where VTE history was absent. Hypertension and dyslipidaemia were overall the most common cardiovascular comorbidities. The burden of depression was highest in PMF with 30.7% of patients reporting a PHQ-9 score ≥ 10. Frailty related outcomes are detailed in Table 2. All four MPNs had high rates of frailty in every domain at baseline. Among Ph- MPNs (ET, PV, and PMF), ET and PV patients generally had a lower burden of frailty compared to PMF patients in most measurements. A high risk of falls as determined by a prolonged get-up-and-go test was present in approximately 20% of PV, CML, and ET patients and 42% of PMF patients. ET patients had the lowest self-reported exhaustion, with less than 40% reporting they ever felt "everything was an effort" or that they "just couldn't get going". PMF patients had the highest self-reported exhaustion. The proportion of patients with low DSST scores was greater in PMF (38.5%) and PV patients (24.3%) than ET (20%) and CML (15%) patients. Unintentional weight loss was common across MPN patients (33.9% to 50%).
Conclusion: There is a high rate of baseline frailty among patients with MPNs with domains differing between diseases. In this cohort, cardiovascular event history at diagnosis was highest among PV patients and lowest in CML patients.
Siegal:Leo Pharma: Honoraria; Novartis: Honoraria; Portola: Honoraria; Bayer: Honoraria; BMS Pfizer: Honoraria. Hillis:Roche: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.